A few of us have been looking into what the correct dose of Fentanyl is for administering the drug via the transmucosal route. I use a ton of Fentanyl in the ER via the IV route and am very comfortable with dosing the drug in this fashion and am starting to use it transnasally, but prior to just about 1 wk ago I had never even considered using the drug transmucosally.
Apparently there are “Fentanyl Lollipops” available in the US (http://www.actiq.com/) which are marketed for managing breakthrough pain in cancer patients, but some literature exists about using this route of administration in battlefield scenarios. As such, when we were considering using this route of administration for my MD Ski Patrol/First Responder pack I was curious as to what was available in Canada. As you may have guessed, the above lollipops are not available in Canada… However, I did find out from a pharmacist that you can get transmucosal Fentanyl tablets which would dissolve as like an sublingual Ativan would.
So… to find a dose I would be comfortable using…. My goal was to figure out what dose of a Fentanyl SL tablet would be useful to have in my pack for both adults and kids if I needed acute pain management and didn’t want to reach for the handy Ketamine. Also, the fact that the drug would be in a tablet form means that I wouldn’t have to worry about it freezing quite as much as I would if carrying a liquid formulation.
This paper:
Evidence-Based Oral Transmucosal Fentanyl Citrate (OTFC) Dosing Guidelines
Lead author: Gerald M. Arnoff
Pain Medicine 2005 Vol 6, #4 pp 305-314
Does a nice job of outlining the how to dose this medication. There are reports of the Fentanyl Lollipops in the dosing rage of 1600 mgr being used, but that sounds like a bit of sledgehammer in my opinion. I want a dose that I can administer to almost anyone I meet on the ski hill/backcountry with a seriously painful injury that I can re-dose as required and not be scared that I also need to carry Narcan with me as this medication only comes in a liquid formulation and again would probably freeze in my pack.
The literature states that when a transmucusal dose of Fentanyl is administered about 25% of the dose is rapid absorbed into the blood stream. Not quite as fast as an IV push dose of course, but the maximum dose effect is probably around the 5 minute range. This is fantastic as you would know if you need to re-dose the medication in a short period of time. The remaining 75% is then absorbed though the gut mucosa and about 25% of the dose actually makes it past hepatic metabolism and into the bloodstream. As such, if I commonly give a patient 1 mgr/kg of IV Fentanyl for analgesia then a 100 kg patient would receive 100 mgr of Fentanyl. As such, I would need to give 4x this dose (as only 25% is absorbed) if I was going to give it transmucosally. Therefore, a 400 mgr dose would be perfect.
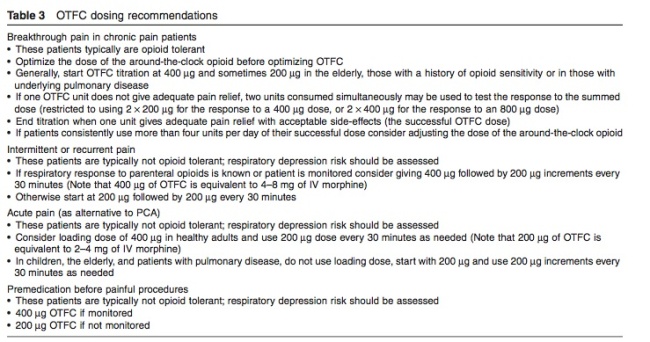
This chart shows that a 400 mgr dose would probably lead to an equivalent dose of 4 – 8 mg of morphine, which seems to be about the perfect dose as a first bolus dose.
This table shows a loading dose of 400 mgr is what the authors recommend and repeating a bolus dose of 200 mgr as required. As such, I am going to get some 200 mgr Fentanyl tabs to have in my pack so that I can give 2 tabs to an adult and 1 tab for a small adult/large child.
Let me know if you have any experience with any of the above or comments.